
The nurses at Surgeon on Site have developed a protocol for patient warming that easily transfers from one clinic to the next. As a traveling service we rely primarily on our own equipment for warming so we know the right equipment is always available, wherever we are.
We recently treated the gorgeous Hugo (6-month-old French Bulldog) for a hindlimb fracture at one of our host practices. Young patients are particularly vulnerable to heat loss and hypothermia, so we wanted to take extra care to keep him warm. The focus on maintaining body temperature starts from admission and continues right through to recovery. Hugo was sitting on a nice thick blanket/vet bed to keep him off the cold kennel floor. After his pre-med injection he was also wrapped in a blanket to prevent excessive heat loss during this time.
A thick blanket/vet bed is placed on the prep table in preparation for induction. We generally avoid using electric heat pads to prevent any risk of burns. After induction we wrap the distal extremities and body in foil blankets, before placing a thick blanket on top.
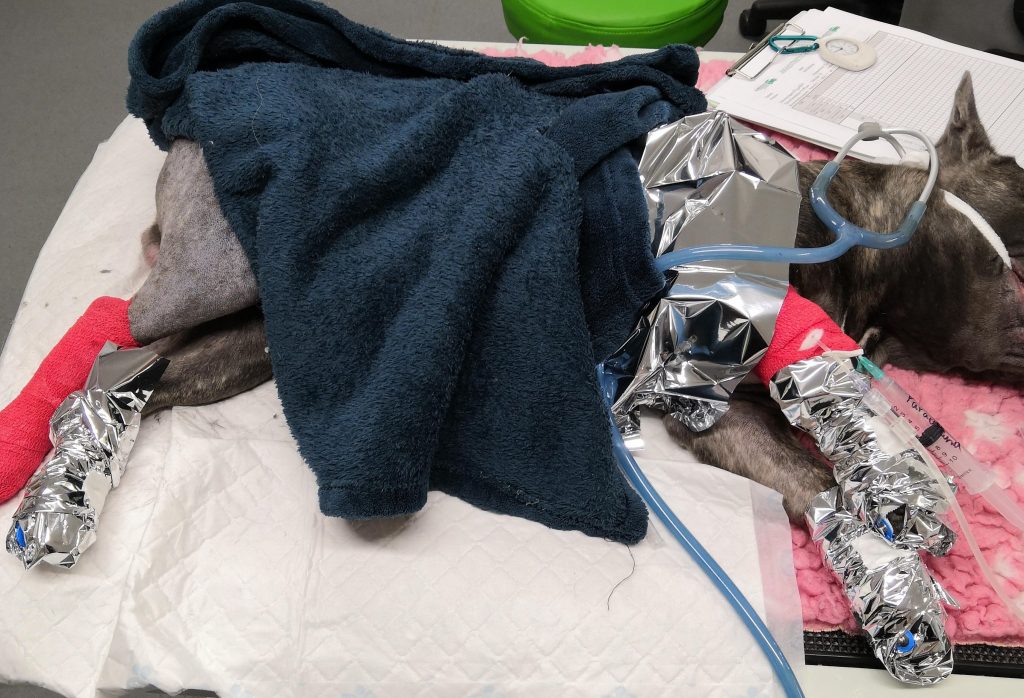
Heat (and fluid) loss from the rapid turnover of dry anaesthetic gases can be quite significant for animals under gaseous anaesthesia. To minimise this cooling effect we use Thermovents® (in-line airway heat exchangers) within the anaesthetic circuit for all of our patients throughout anaesthesia.

The theatre table was pre-warmed prior to induction. Some of our host clinics do have tables with integrated warming, but we also place a thick blanket on the table followed by the Bair Hugger™ blanket. This is switched on at 38°C and left in place until we need to transfer the patient from the prep area to theatre.
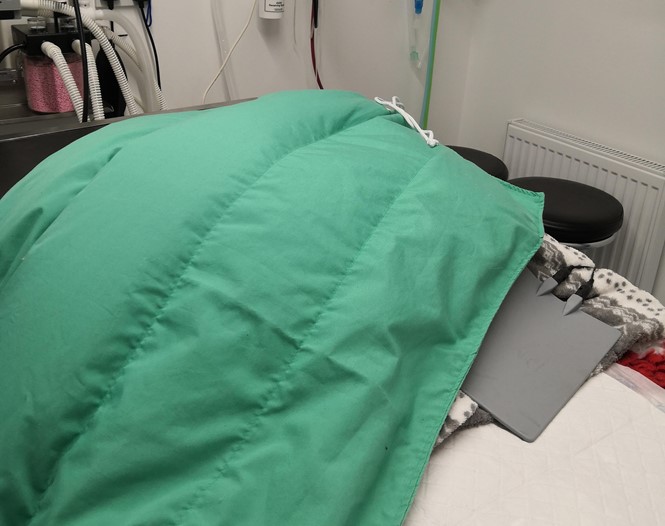
Hugo was positioned on the theatre table ready for surgery, with the Bair Hugger™ blanket on top of his body and a blanket placed on top. Large surgical drapes were placed to cover his entire body and help to trap warm air. The surgeons prefer that the Bair Hugger is not started until the patient is draped. Every patient is monitored using an oesophageal temperature probe with their temperature visible on our multi-parameter monitor screen throughout surgery. Not all patients will require the Bair Hugger to be switched on, and it is important to avoid overheating the patient. By monitoring the temperature throughout we can decide when to switch it on and at what setting.
Hypothermia during and after surgery is associated with a number of different complications including delayed anaesthetic recovery, increased risk of surgical infection, shock and reduced blood clotting. A patient that has remained normothermic throughout their procedure will have a better recovery and be ready to be discharged back to their owner nice and quickly after their big day.
For further reading, please use the links below.
httpss://todaysveterinarypractice.com/focus-on-hypothermia-operating-room/
Surgeon on Site | ©2022 | All Rights Reserved.